PatellaFemoral Pain Syndrome (PFPS)
What is Patellofemoral Pain Syndrome?
Patellofemoral pain syndrome (PFPS), also known as “runner’s knee”, is a broad term that describes pain in the front of the knee and around the kneecap. It’s one of the most common overuse injuries of the knee. Although it’s more common in individuals that participate in sports with lots of running or jumping, it can occur in nonathletes as well.
Background
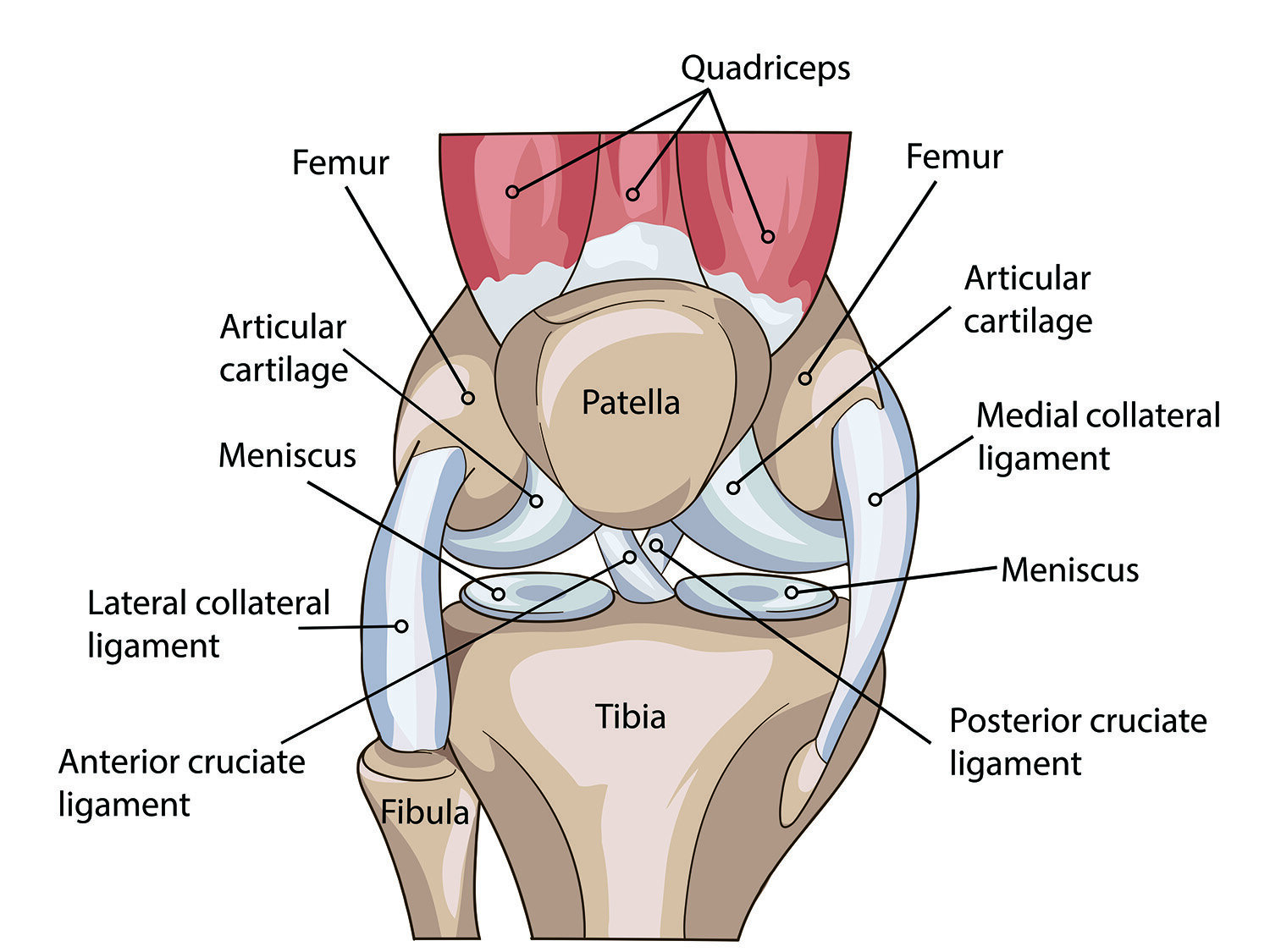
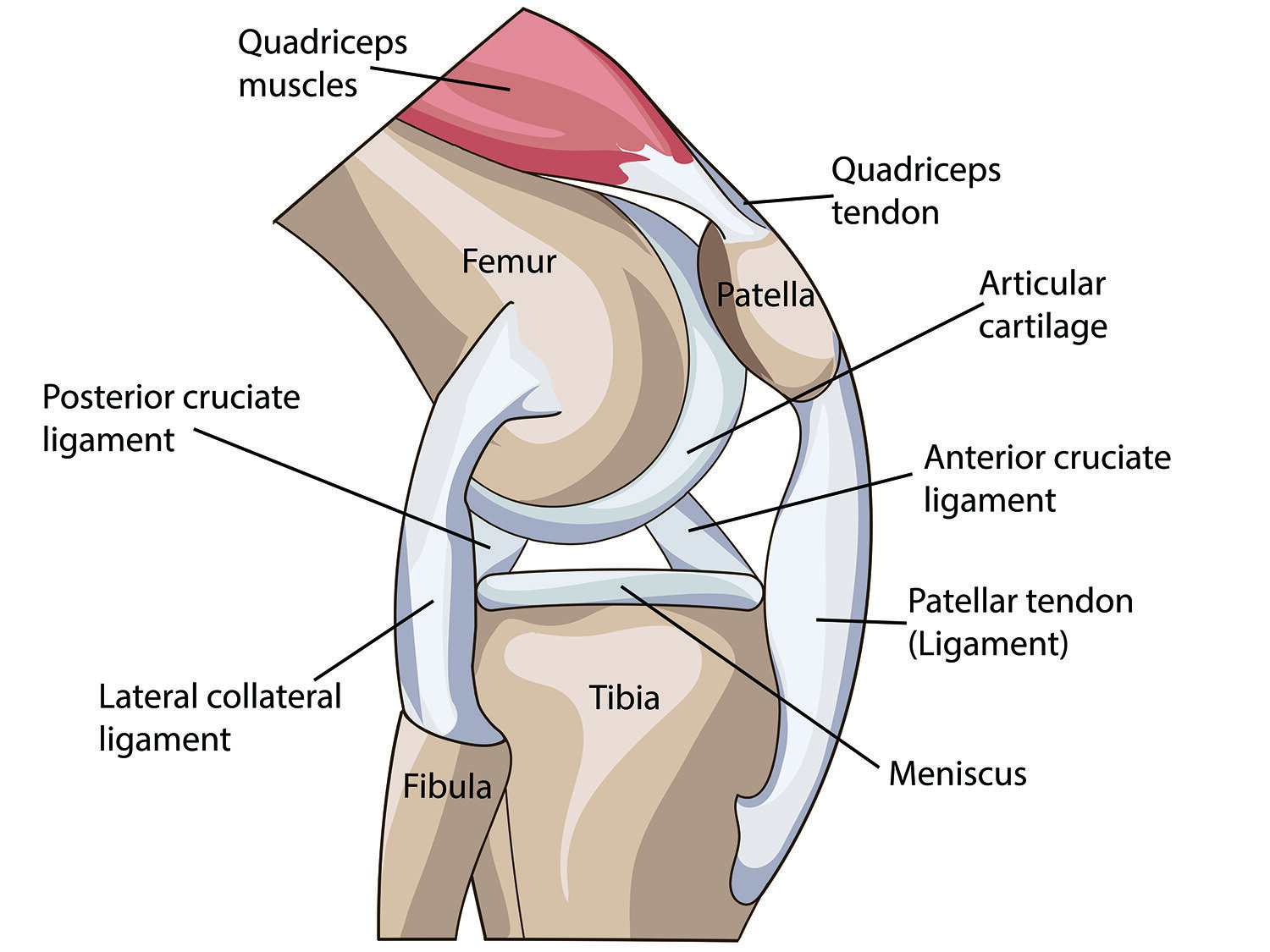
The knee joint is made up of several structures. The lower end of the femur (thigh bone) interacts with the upper end of the tibia (shin bone) and the patella (kneecap). These bones are connected to each other with several ligaments, and the entire joint is surrounded by connective tissue and muscles. For example, the patellar tendon connects the quadriceps muscles on the front of your thigh to the top of your tibia, going up and over the patella to use it as a pivot point. As the name indicates, patello-femoral pain syndrome focuses on the interaction between the femur and the patella. When you bend or straighten your knee, the patella glides smoothly along the lower end of your femur. A thin layer of cartilage-- both on the underside of your patella and on the corresponding groove on your femur-- helps the bones glide smoothly against each other during this movement.
What Causes Patellofemoral Pain Syndrome?
Several things may contribute to the development of PFPS, including overload, muscle imbalance or weakness, movement coordination deficits, or mobility problems in adjacent structures.
Overload:
In many cases, a rapid change in frequency or intensity of activity can result in an overuse injury. Some specific movements-- running, squatting, or climbing stairs-- put higher loads through the knee. Although these movements are a component of normal daily life, overuse injuries occur when the amount of load through the joint exceeds the tissue’s ability to recover on a timely basis.Muscle imbalance:
The quadriceps are a key muscle group for the patellofemoral joint, since the associated patellar tendon goes directly over the kneecap. Weak quadriceps or strength imbalances compared to other muscle groups can cause poor tracking of the patella on the femur, resulting in abnormal “wear and tear” and pain.Movement coordination:
In addition to muscle imbalance, poor motor control can also alter biomechanics at the knee. For example, inward movement of the knee during a squat is associated with PFPS.Mobility deficits:
Increased mobility at adjacent joints (in the hip or foot) and/or decreased flexibility in the muscles or connective tissues surrounding the knee joint may also alter mechanics and cause pain in specific movements.
Factors that can increase your risk of PFPS include:
Age:
PFPS typically affects adolescents and young adults, especially those who participate in sports with lots of running or jumping.Sex:
Women are twice as likely as men to develop PFPS due to differences in pelvis width, which affect the mechanics of the knee joint.Sports:
Runners and jumping athletes may experience increased stress through their knees, especially in cases with overtraining, poor technique or equipment, or recent changes in playing surface. An appropriate training plan can help reduce this risk.
Common Symptoms
PFPS is an umbrella term that describes a group of symptoms that consistently occur together. The most common symptom is dull, achy pain in the front of your knee. This may be aggravated by squatting, kneeling, running, jumping, sitting for a long period of time, or going up or down stairs. Other common symptoms include:
Stiffness
Swelling
Popping or crackling sensations
Weakness
How Can Physical Therapy Help?
Physical therapy can get you back on your feet and on the road to recovery, even with chronic or severe knee pain. Due to the many root causes of PFPS, treatment is unique to the individual. Treatments may include:
Gait and movement retraining to improve the dynamic alignment of your knees, so that you can better perform activities including squatting, kneeling, walking, running, jumping, and climbing stairs
Strength training targeting quadriceps muscles and other key groups for knee stabilization, including your glutes and core
Stretching and soft tissue mobilization to increase flexibility of your iliotibial (IT) band, quadriceps, hamstrings, and calf
Manual therapy and taping to directly address patellar tracking
Footwear and orthoses to support improved alignment of your knees and lower extremities during daily activities and sport-related movement
Ice, active recovery, and appropriate rest to reduce pain and inflammation at the knee joint
AUTHOR:
Katie Hutchins, PT, DPT
LWPT Kirkland Physical Therapist
CONTRIBUTORS:
Dr. Ghislaine Robert, MD
Sport & Spine Physician
Dr. Bob Adams, DO
Ret. USA Track & Field Head Medical Doctor, Sports Medicine Physician
Ben Wobker, PT, MSPT, CSCS, CFSC, SFMA
Founder & Director Lake Washington Physical Therapy
MORE WEBINARS
MORE BLOGS
References
Patellofemoral Pain Syndrome. Mayo Clinic. 2018. Web. https://www.mayoclinic.org/diseases-conditions/patellofemoral-pain-syndrome/symptoms-causes/syc-20350792
Patellofemoral Pain Syndrome. OrthoInfo: American Academy of Orthopedic Surgeons. 2020. Web. https://orthoinfo.aaos.org/en/diseases--conditions/patellofemoral-pain-syndrome
Patellofemoral Pain: Clinical Practice Guideline. Journal of Orthopedic Sports Physical Therapy. 2019; 49(9): CPG1–CPG95. doi:10.2519/jospt.2019.0302. https://www.jospt.org/doi/full/10.2519/jospt.2019.0302#_i126