Plantar Fasciitis
What is Plantar Fasciitis?
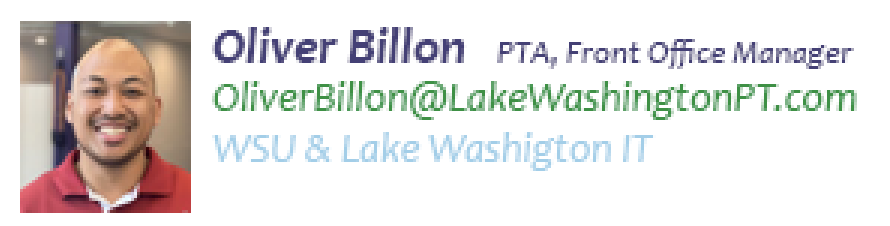
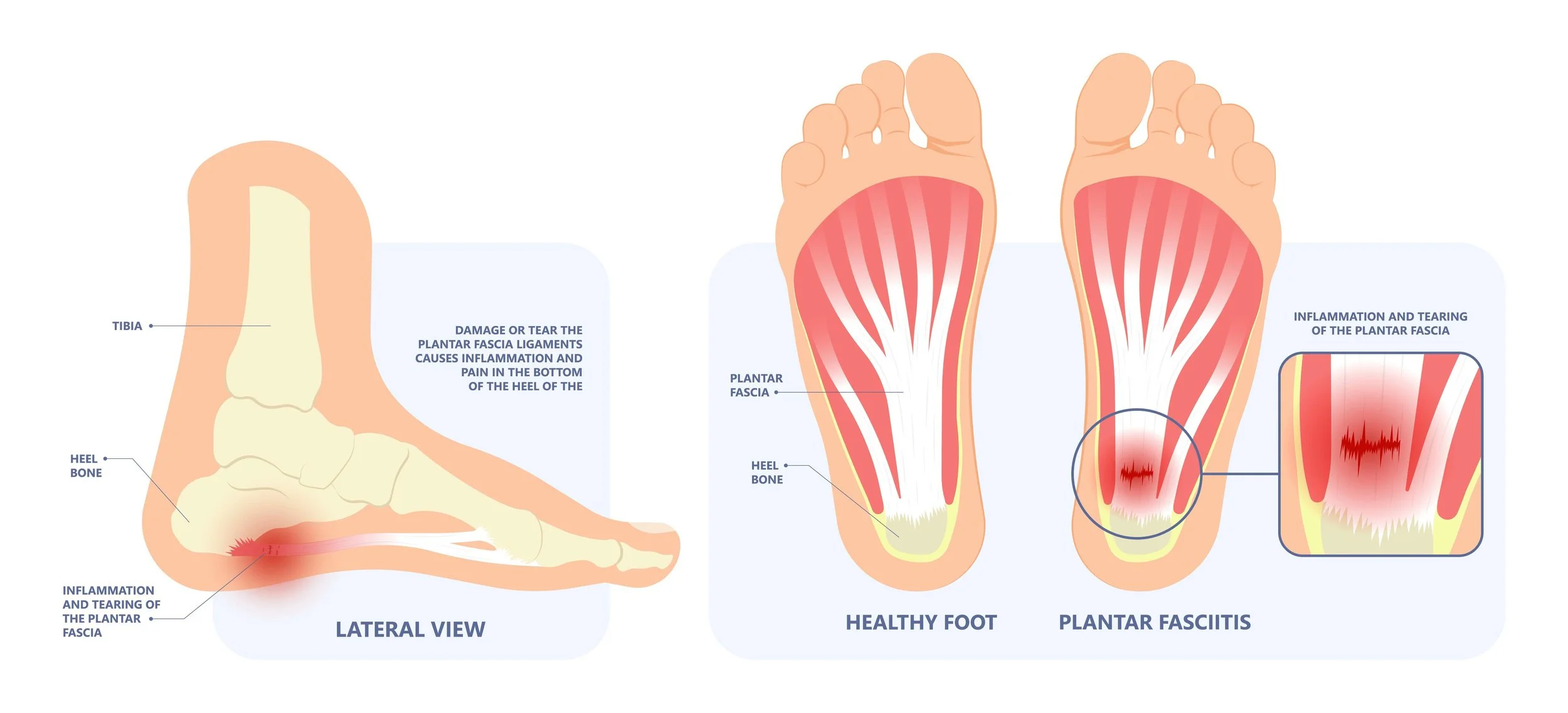
The plantar fascia is a thick band of connective tissue that runs from the bottom of your heel to the ball of your foot. It is one of the structures that supports the arch of your foot, and it acts as a shock absorber as you stand, walk, and run. Plantar fasciitis is an inflammation of the plantar fascia that results in a deep stabbing pain in the heel, especially first thing in the morning and after standing for extended periods of time. Plantar fasciitis is a common overuse injury in people who spend a lot of time on their feet, and especially in runners. It is sometimes associated with specific foot structures such as flat feet or high arches, and may be associated with a tension in the Achilles tendon or calf muscles.
What are the Early signs of Plantar Fasciitis?
Pain or burning sensation in the heel or the bottom of the foot
Discomfort and stiffness especially in the morning or after sitting for a long time.
Stiffness in the foot, especially in the heel area.
Tenderness in the heel or arch area when touched.
Swelling or redness in the heel area.
Pain that worsens after standing, walking or running for long periods of time.
Heel pain that can vary from deep stabbing pain to diffuse aching through the arch of the foot
Tends to improve with moderate activity, i.e. “warming up” into a walk
Can develop gradually over time, and may be a chronic condition with intermittent acute flare-ups.
““Believe me, when I say this, I do get a sensation at the bottom of my heel and crosses multiple joints of my foot.”
”
What Causes Plantar Fasciitis?
Several things may contribute to the development of plantar Fasciitis, including many but not limited to the following:
Plantar Fasciitis is caused by various factors, including:
Overuse: Repetitive activities, such as running, jumping, or standing for long periods of time, can put excessive stress on the plantar fascia, leading to inflammation and pain.
Bone Spurs: often there is a boney protuberance or spur that forms near the base of the heel that can deform, push, poke, and tear the proximal attachment of the plantar fascia
Age: As people get older, the plantar fascia can become less elastic, making it more susceptible to injury.
Weight: Excess body weight puts additional stress on the feet, including the plantar fascia.
Foot structure: High arches, flat feet, or tight Achilles tendons can affect the way weight is distributed across the foot, leading to increased stress on the plantar fascia.
Shoes: Wearing shoes that do not provide adequate support or cushioning can also lead to plantar fasciitis.
Certain medical conditions: Certain conditions, such as obesity, rheumatoid arthritis, or diabetes, can increase the risk of developing plantar fasciitis.
What does the Plantar Fascia Do?
The plantar fascia acts as a shock absorber when walking and provides arch support, especially at the midtarsal joint. Think of pushing play-doh down and it expands on the floor.
Quick Gait Review:
First contacting the ground: When walking you need to demonstrate the ability of your foot/ankle to collapse to allow for shock absorption and be able to transition into a rigid stable lever in order to propel yourself in walking.
After contacting the ground: After the phase of the whole foot contacting the ground, your subtalar joint as presented above in fig 1, your subtalar joint needs to invert prior to heel lift while we are still in an everted position which acts as a rigid lever which forces the 1st metatarsal to perform toe extension for proper push-off.
When Orthotics are involved we need to look “functionally” at how it looks while you ambulate. When orthotics that is supposed to “mold” into your foot/ankle to assist especially those who are considered “flat feet”. Some individuals may start to overly supinate their foot/ankle overtime which may cause a change in their foot/ankle biomechanics. It is hard to change someone’s walking mechanics when you have been walking like that pretty much your whole life.
How long does plantar fasciitis last?
The duration of plantar fasciitis can vary greatly, depending on several factors such as the severity of the condition, the individual's overall health, and the effectiveness of treatment. For some people, plantar fasciitis can resolve within a few months with proper care and physical therapy. However, for others, it can persist for a year or longer and may become a chronic condition if left untreated. Effective treatment and management are important for reducing the duration of plantar fasciitis and promoting healing.
You should notice your plantar fasciitis symptoms incrementally improve as soon as you begin physical therapy. But it can take anywhere from a few weeks to a few months for your plantar fascia to be completely resolved. For many clients there is continual maintenance and precautions that should be relatively observed to avoid it coming back.
How Can Physical Therapy Help?
Physical therapy can get you back on your feet and on the road to recovery, even with chronic or severe knee pain. Due to the many root causes, treatment is unique to the individual case. Treatments may include:
Ice, active recovery, and appropriate rest to reduce pain and inflammation at the heel or medial arch
Manual therapy techniques for symptom relief directly at the plantar fascia and surrounding musculature and associated hydration
Strengthening the “intrinsic” foot muscles which support the arch
Balance training to improve control of the foot/ankle to offload the overloaded structures
Stretching and mobility strategies to provide relief of surrounding tension in the muscles and tendons
Gait and movement retraining to improve the dynamic alignment of your knees, hips, and ankles, so that you can better perform activities including squatting, kneeling, walking, running, jumping, and climbing stairs
Strength training targeting quadriceps muscles and other key groups for knee stabilization, including your glutes and core
Footwear and orthoses to support improved alignment of your knees and lower extremities during daily activities and sport-related movement
Taping techniques to offload the plantar fascia throughout the day
Further treatment may also include physician-administered corticosteroid injections, shockwave therapy, or other options as appropriate
““There may be an issue where your foot/ankle does not allow for quicker pronation “flattening of the arch”, which can cause you to stay lateral on your gait mechanics which may cause stress to your knees as well. I’ve seen a lot of this in the clinic and it does take time for your foot to adapt.””
What Can I do Immediately at Home?
Relative rest - maintain a threshold of activity without exacerbating your symptoms by changing the frequency, intensity, or even modifying the technique of the aggravating movements
Warm up activities to start the day - stretches and active movement before you put your feet on the ground in the morning
Myofascial/soft tissue massage - rolling a “spiky ball” on the arch of the foot throughout the day can provide a similar (though less intense) relief to in-clinic techniques
Usually available in running stores, or online as a “Pro Tec spiky ball” or similar
Ice massage at the end of the day or when aggravated - 5-10 min at the area of pain, as needed
Supportive footwear - good arch support 100% of the time, including inside the house
Orthotics - over the counter (Superfeet) or even custom-fitted orthotics can add additional arch support in your selected supportive footwear
AUTHORs:
Katie Hutchins, PT, DPT
LWPT Kirkland Physical Therapist
Oliver Billon, PTA
LWPT Redmond Physical Therapist Assistant
CONTRIBUTORS:
Dr. Ghislaine Robert, MD
Sport & Spine Physician
Dr. Jonathan Hall, MD
Foot & Ankle Orthopedic Surgeon
Dr. Bob Adams, DO
Ret. USA Track & Field Head Medical Doctor, Sports Medicine Physician
Ben Wobker, PT, MSPT, CSCS, CFSC, SFMA
Founder & Director Lake Washington Physical Therapy
MORE WEBINARS
MORE BLOGS
References
American Association of Orthopaedic Surgeons. Plantar Fasciitis and Bone Spurs. (https://orthoinfo.aaos.org/en/diseases--conditions/plantar-fasciitis-and-bone-spurs) Accessed 11/4/2022.
American College of Foot and Ankle Surgeons. Plantar Fasciitis. (https://www.foothealthfacts.org/conditions/plantarfasciitis) Accessed 11/4/2022.
U.K. National Health Service. Plantar Fasciitis. (https://www.nhs.uk/conditions/plantar-fasciitis/) Accessed 11/4/2022.
U.S. National Library of Medicine. Plantar Fasciitis. (https://medlineplus.gov/ency/article/007021.htm) Accessed 11/4/2022.