What Is Little League Elbow?
Chances are that you have heard the term Little League elbow. Most have encountered it in the media, during youth playing days, or from their own children. As a medical provider specializing in youth throwing and overhead athletes (baseball, softball, tennis, etc.), I’d like to provide some clarity around something that is commonplace yet poorly understood. This article answers the questions: What is Little League elbow? What causes it? How do you treat it? How is it prevented?
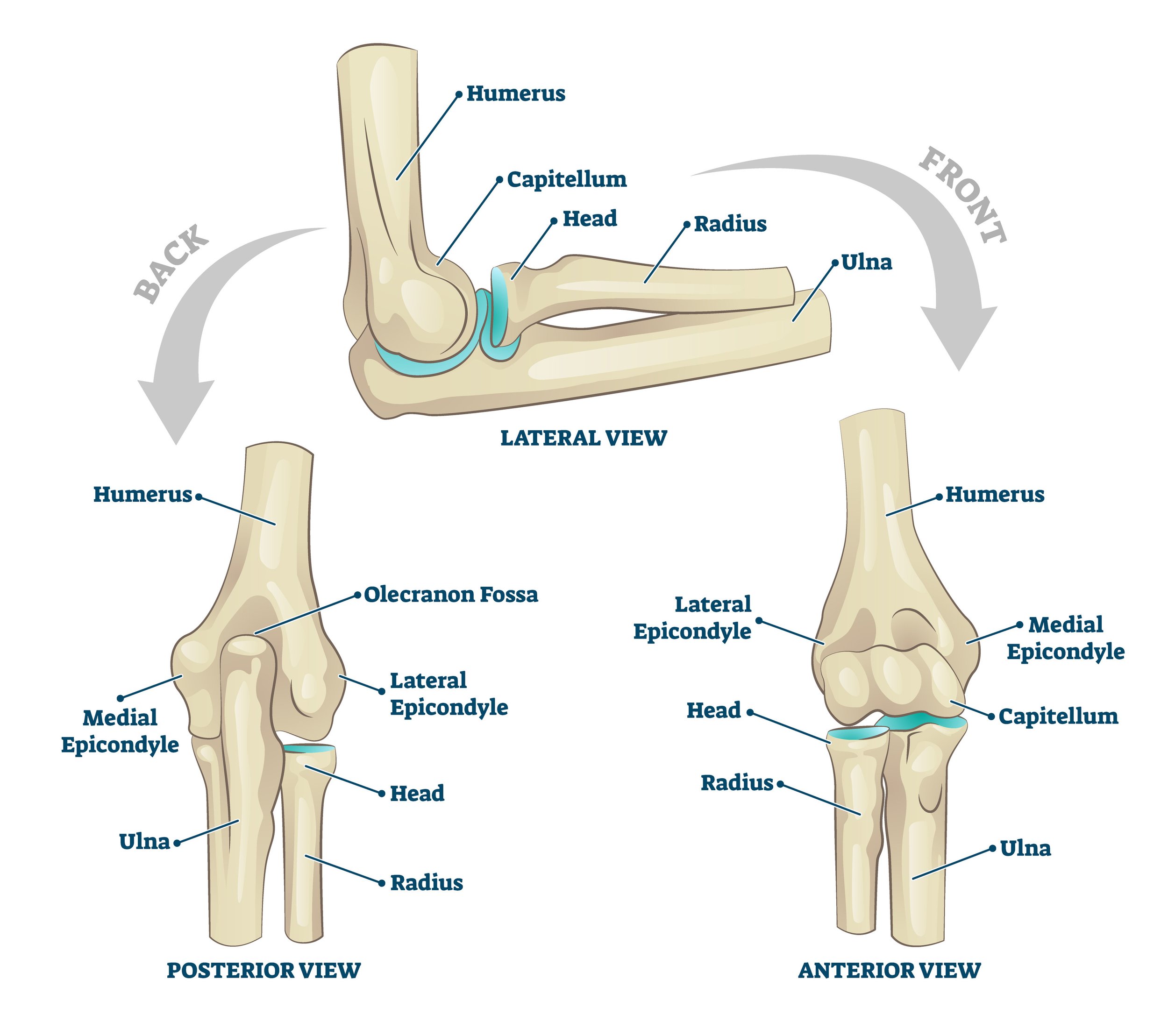
Medial Elbow Anatomy: The Basics
To understand what Little League elbow (LLE) is, you need a rough grasp of the complex anatomy of the medial elbow. Below is an abbreviated list of the relevant structures that play a role in LLE.
Bones:
Medial Epicondyle: The large bone felt on the inside of the elbow. It is the attachment site for the forearm/finger muscles that make a fist and flex your wrist. The ulnar collateral ligament (see below) also attaches here.
Medial Epicondyle Apophysis (growth plate): The growth plate located on the medial epicondyle at the inside of the elbow. This is the structure injured in LLE.
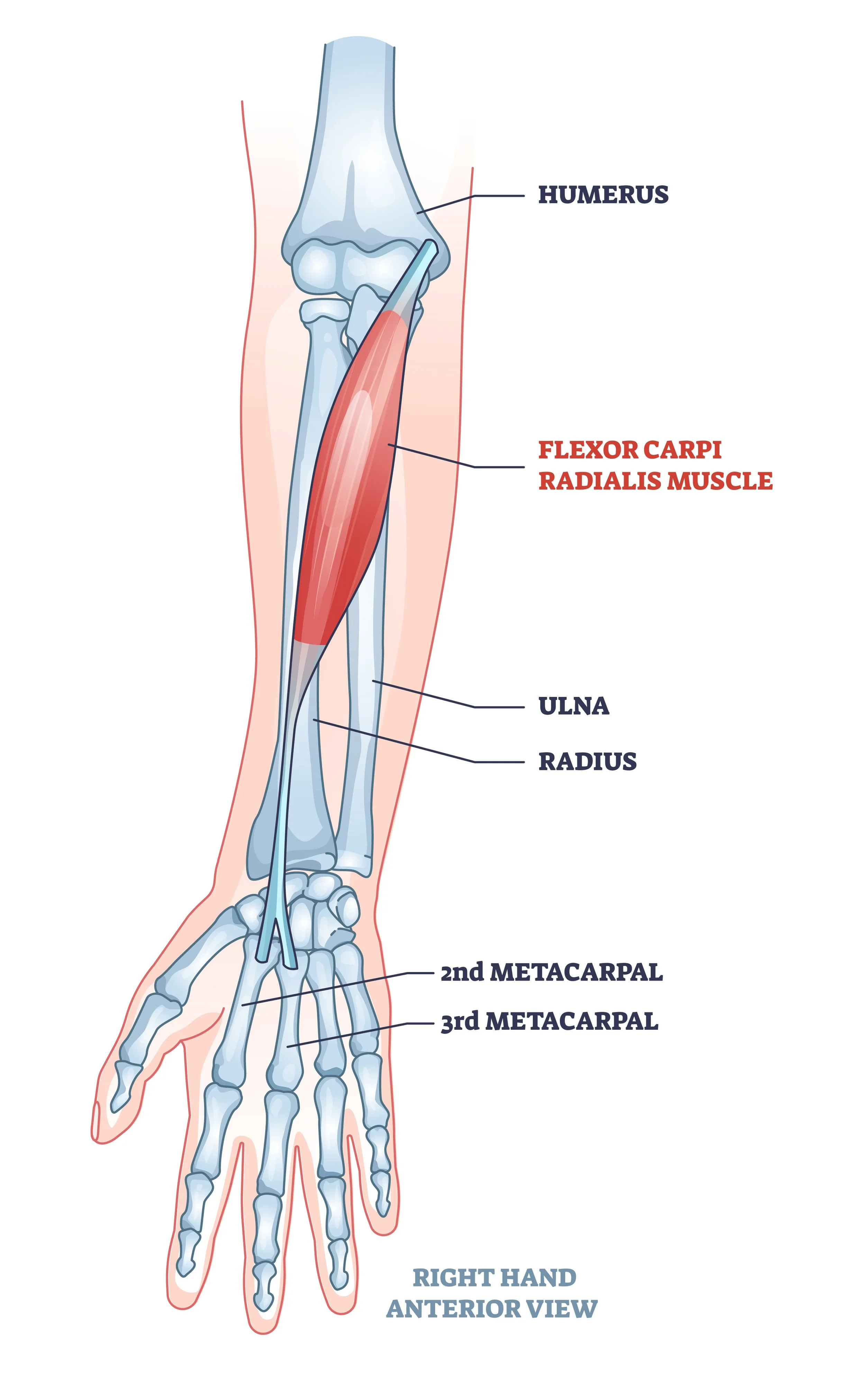
Muscles:
Wrist/Finger Flexors: The group of muscles in charge of flexing the wrist and fingers (heavily utilized during the throwing motion).
Common Flexor tendon: The tendon that connects the flexor muscle group to the inside elbow (medial epicondyle).Ligaments:
Ulnar collateral ligament (UCL): aka the Tommy John ligament. The ligament that helps hold the elbow together and connects the upper and lower arm bones. This is the ligament commonly injured in adult pitchers, but less commonly involved in youth athletics and Little League elbow. It is heavily stressed during the throwing motion.
““Too much stress can lead to injury, stress is a product of power and power is necessary for progression in baseball”.
”
What Is Little League Elbow?
Little League elbow is an injury to the growth plate on the inside (medial) elbow of a throwing athlete. It includes various levels of pathology.
Medial epicondyle apophysitis: Irritation and inflammation (without fracturing) of the growth plate on the inside elbow.
Medial epicondylar avulsion fracture: Fracturing and separation of the bone in the medial elbow from its growth plate. An avulsion fracture usually starts out as apophysitis (see above) and evolves into fracturing when not properly treated or if continued throwing takes place.
Flexor tendinopathy (aka golfer’s elbow): Flexor tendinopathy is not technically a Little League elbow diagnosis. However, it is often lumped into the term Little League elbow and can be seen as one of its initial stages. It is irritation of the tendon that connects the wrist flexors (the muscles that make a fist) to the inside of the elbow. If the athlete continues to throw through pain, the tendinopathy can turn into one of the above-listed pathologies and may become Little League elbow.
““Acute elbow pain or even slow developing pain is something that should be looked at by a physical therapist or elbow specialist.””
What Causes Little League Elbow?
Little League elbow is an overuse injury that does not have a single causal factor. It primarily occurs in young athletes ages 8-15 years old. It results from several factors that culminate to create stress levels in the elbow that are too great for the athlete's musculoskeletal system to handle. The best answer to the question of what causes Little League elbow is:
Excessive throwing volume
Throwing intensity
Poor workload management.
Additional factors that are often mentioned in the etiology of Little League elbow:
Pitch Type
It has long been believed that throwing curveballs from a young age can cause Little League elbow. This is not the case. Throwing too much of any pitch type can create elbow pathology. Many recent studies have shown that fastballs create greater stress levels in the medial elbow than curveballs. It is not the curveball’s fault.
Throwing Mechanics
Throwing mechanics may play a role in the development of Little League elbow, but they do not cause it.
Athletes that are new to baseball and have terrible “pitching mechanics” can develop Little League elbow. So can little Johnny, who has played since he learned to walk and has the best arm action in the league.
Throwing of any kind causes stress to the elbow. If an athlete's workload management is poorly monitored and these stress levels become too great for the elbow to handle, pain can develop. This is true regardless of whether the athlete has the best or worst mechanics.
Yes, studies have shown that poor throwing mechanics can lead to increased torque/stress on the medial elbow. However, studies also show that throwing hard in and of itself increases elbow stress/torque. Therefore, the harder a kid throws and the better the kid gets at baseball, the more stress he will create in his elbow. It is not uncommon to see the player with the best mechanics, who also throws the hardest, develop LLE—especially if this player is used most often for pitching and playing shortstop or other positions with high throwing demands.
Young athletes generally have poor throwing form. As athletes progress in their sport/age, their pitching mechanics tend to improve. This means you should not stress if your Little Leaguer has bad form—that's what the youth leagues are for! This is the time the athlete is learning and shaping their arm to improve the efficiency with which they throw.
Fatigue
A single day of throwing when the athlete did not sleep well or has fatigue from a long day at school does not lead to LLE. However, repeatedly throwing through this fatigue, lack of sleep, or overexertion throughout multiple sports may very well increase the risk of LLE.
““It is critical for the athlete have honest communication with the coach as this is the greatest prevention of season ending injuries.””
How Do You Treat LIttle League Elbow?
Little League elbow is primarily treated with rest and reduced throwing volume/intensity. The athlete must reduce aggravating factors and allow for the elbow tissue to heal. This treatment may look different for the various types of LLE pathology.
For example:
If the athlete presents with no concrete separation of the growth plate or with a diagnosis of wrist flexor tendinopathy, then they can usually continue playing baseball with modified activity. Pitching and catching are typically out of the picture; however, positions such as first base and designated hitter are great alternatives. Second base and outfield with strict instructions on hitting the cut-off are also viable options depending on the severity of the case.
When clear and significant growth plate separation has occurred, or the athlete has suffered from an avulsion fracture, strict rest and avoidance of throwing is necessary (usually a minimum of 4-6 weeks). Additional steps may be taken, such as casting, splinting, or even surgery.
““A kinetic chain that is dysfunctional will eventually injure the shoulder or elbow.””
How Do you Prevent LIttle League Elbow?
No one can guarantee the prevention of Little League elbow. There are ways, however, to lessen the chance of developing elbow pain.
Practice proper arm care, including warming up and cooling down.The warm-up should increase the athlete’s heart rate, get blood flowing, and cause a light sweat. It should include movements that work the rotator cuff and shoulder blade but do not completely fatigue these muscles. The cool-down should be similar to the warm-up and should work the athlete’s throwing arm to help promote fluid return and muscle activation. The cool-down should not consist of wrapping the arm in ice and sitting still.
Manage the workload and monitor throwing amounts.The single best way to prevent Little League elbow is to avoid overuse and over-throwing. Workload management is a complex equation involving the volume of throws, the intensity of throws, and the frequency with which they are performed. It involves something called the acute:chronic workload ratio.
Acute:Chronic workload ratioT
his is a ratio that essentially compares how much an arm throws in a single outing to how accustomed that arm is to throwing over time. For example, if I am used to running 1 mile three times per week (chronic), then one day go out and try to run 10 miles in one outing (acute) I may get hurt. This large spike in acute stress far exceeds the chronic workload that I am accustomed to and can increase my risk of injury. This is why pitchers should have a gradual progression of throwing over time (think weeks, not days) before putting them on the mound for high-intensity throwing.
If you are not up to speed on the complex topic of acute:chronic ratios, then pitch counts can be a good tool for managing workload.
DON'T THROW THROUGH PAIN!Throwing is a violent motion that puts extreme amounts of strain on the athlete's arm. Don’t freak out if little Johnny has one or two days of pain after a long outing. This is common. However, don’t have little Johnny push through pain or throw with continued pain for long periods of time. I recommend seeing a medical provider, such as a baseball-specific physical therapist, if throwing pain persists for 1-2 weeks or longer.
How Can Physical Therapy Help Little League Elbow?
Although rest and reduction in throwing is the primary treatment for Little League elbow, physical therapy is a highly recommended supplement to the recovery process. During rehabilitation, physical therapy can help improve the strength of the muscles involved in throwing, such as the wrist flexors, rotator cuff, scapular stabilizers, and the core. Not only can this help prevent atrophy during times of disuse, but it may also help reduce stress levels to the injured elbow once throwing is resumed. Additionally, a baseball-specific PT can help with a safe return to throwing. A proper return-to-throw program will provide the athlete with a safe yet efficient path to high-intensity throwing without running the risk of overexerting the freshly healed elbow.
Bottom Line
Little League elbow is an injury to the medial elbow of youth throwing athletes. It can range from tendinitis to growth plate irritation to full-blown fracture.
Little League elbow is caused by poor workload management through excessive throwing volume, throwing intensity, or inadequate rest and recovery. It is not caused by bad mechanics, curve balls or muscle weakness.
Little League elbow is primarily treated with rest and a reduction in throwing. However, steps such as physical therapy and sport modification can play a role in allowing continued participation and quicker recovery.When considering PT for a baseball/softball injury, I recommend seeing someone who specializes in overhead athletes and throwing sports.
About the Author:
Jordan Bork (PT, DPT, CSCS, CFSC) is an orthopedic and sport physical therapist who specializes in overhead athletes and baseball/softball rehabilitation. He works full-time at LWPT Kirkland and part-time at Driveline Baseball in Kent. Jordan treats patients of all competitive levels, including professional and college; however, his passion is in youth athletics ranging from Little League to high school.
AUTHOR:
Jordan Bork, PT
Physical Therapist and Baseball Specialist
CONTRIBUTORS:
Terry Phillips, PT, DPT
Physical Therapist and Baseball Specialist
Joe Midgett, PT, DPT
Physical Therapist and Baseball Specialist
Bob Adams, DO
Sports Medicine Physician and Former head of the medical team for USATF
Avi Goodman, MD
Evergreen Health Orthopedics & Sports Medicine
Vincent Santoro, MD (Retired)
Orthopedic Surgeon and former college pitcher
Ben Wobker, PT, MSPT, CSCS, CFSC, SFMA
Founder & Director LWPT
MORE BLOGS
MORE WEBINARS
REFERENCES
Chandra, Venita, et al. “Thoracic Outlet Syndrome in High-Performance Athletes.” Journal of Vascular Surgery, vol. 58, no. 2, 2013, pp. 567–568., doi:10.1016/j.jvs.2013.05.086.
Ferrante, Mark A., and Nicole D. Ferrante. “The Thoracic Outlet Syndromes: Part 2. The Arterial, Venous, Neurovascular, and Disputed Thoracic Outlet Syndromes.” Muscle & Nerve, vol. 56, no. 4, 2017, pp. 663–673., doi:10.1002/mus.25535
Hangge, Patrick, et al. “Paget-Schroetter Syndrome: Treatment of Venous Thrombosis and Outcomes.” Cardiovascular Diagnosis and Therapy, vol. 7, no. S3, 2017, doi:10.21037/cdt.2017.08.15.
Otoshi, Kenichi, et al. “The Prevalence and Characteristics of Thoracic Outlet Syndrome in High School Baseball Players.” Health, vol. 09, no. 08, 2017, pp. 1223–1234., doi:10.4236/health.2017.98088.
Sanders, Richard J, et al. “Diagnosis of Thoracic Outlet Syndrome.” Journal Of Vascular Surgery, vol. 46, no. 3, Sept. 2007, pp. 601–604., www.sciencedirect.com/science/article/pii/S0741521407007343.
Thompson, Robert W. “Thoracic Outlet Syndrome and Neurovascular Conditions Of The Shoulder In Baseball Players.” Baseball Sports Medicine, by Christopher S. Ahmad and Anthony A. Romeo, Wolters Kluwer, 2019.
Watson, L.a., et al. “Thoracic Outlet Syndrome Part 1: Clinical Manifestations, Differentiation and Treatment Pathways.” Manual Therapy, vol. 14, no. 6, 2009, pp. 586–595., doi:10.1016/j.math.2009.08.007.
Watson, L.a., et al. “Thoracic Outlet Syndrome Part 2: Conservative Management of Thoracic Outlet.” Manual Therapy, vol. 15, no. 4, 2010, pp. 305–314., doi:10.1016/j.math.2010.03.002.
Popkin, C. A., Bayomy, A. F., & Ahmad, C. S. (2019). Early Sport Specialization. Journal of the American Academy of Orthopaedic Surgeons, 27(22), e995–e1000.
DiFiori JP, Benjamin HJ, Brenner JS, et al. (2014) Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. British Journal of Sports Medicine; 48:287-288.
Post EG, Trigsted SM, Riekena JW, Hetzel S, McGuine TA, Brooks MA, Bell DR. (2017). The Association of Sport Specialization and Training Volume with Injury History in Youth Athletes. Am J Sports Med; 45(6):1405-1412. doi: 10.1177/0363546517690848.
Buckley PS, Bishop M, Kane P, Ciccotti MC, Selverian S, Exume D, Emper W, Freedman KB, Hammoud S, Cohen SB, Ciccotti MG. (2017). Early Single-Sport Specialization: A Survey of 3090 High School, Collegiate, and Professional Athletes. Orthop J Sports Med. 28;5(7)
Bell DR, Post EG, Biese K, Bay C, Valovich McLeod T. (2018). Sport Specialization and Risk of Overuse Injuries: A Systematic Review With Meta-analysis. American Academy of Pediatrics; 142(3)
Myer, G. D., Jayanthi, N., DiFiori, J. P., Faigenbaum, A. D., Kiefer, A. W., Logerstedt, D., & Micheli, L. J. (2016). Sports Specialization, Part II: Alternative Solutions to Early Sport Specialization in Youth Athletes. Sports health, 8(1), 65–73.
Disclaimer: The information listed on this page is not to be used as medical advice. If you have any questions or concerns regarding stretching, mobility, or strength training, please seek out professional attention.