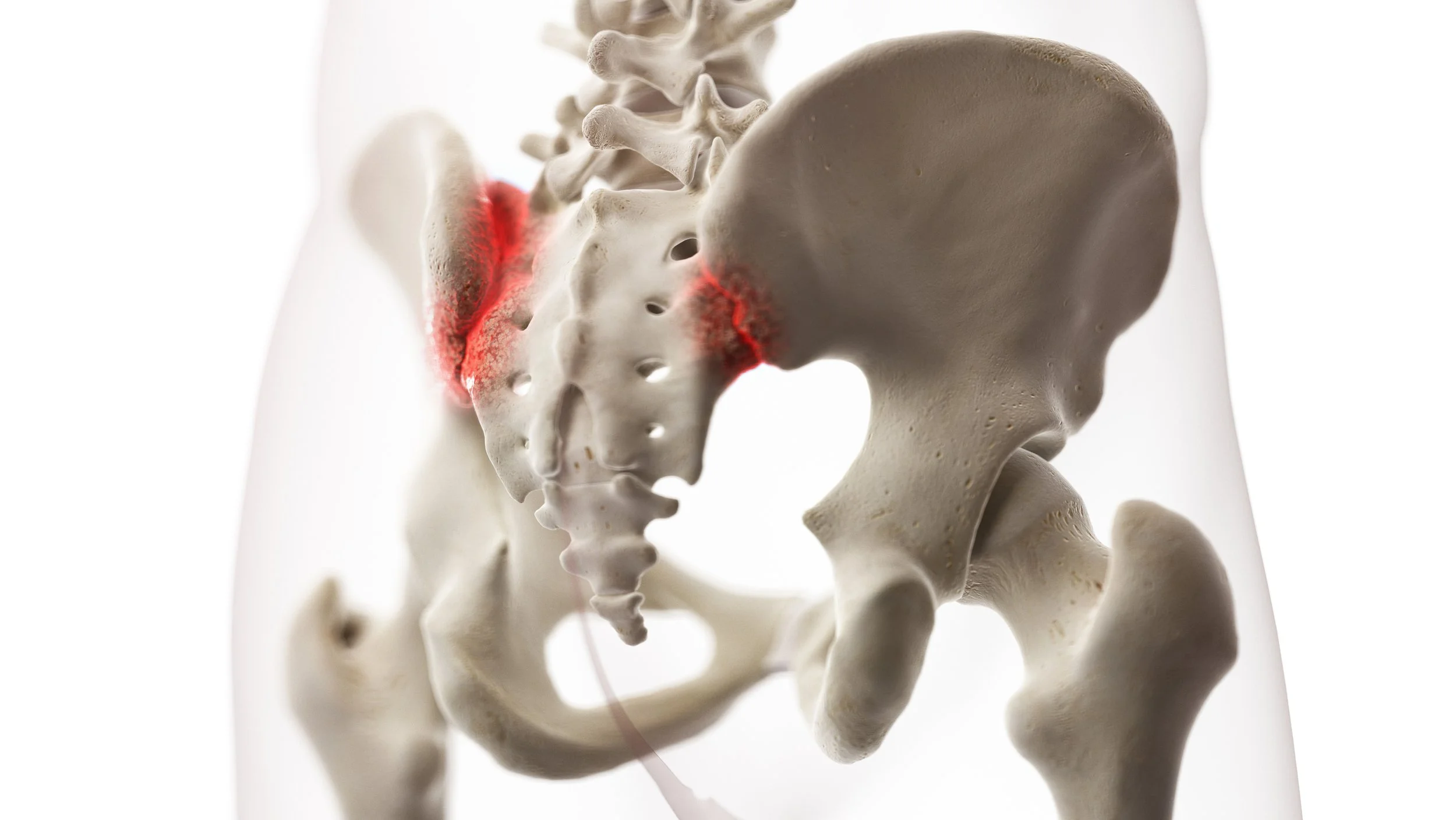
What is the SI Joint?
The SI Joint
An anatomical review of the Sacroiliac Joint
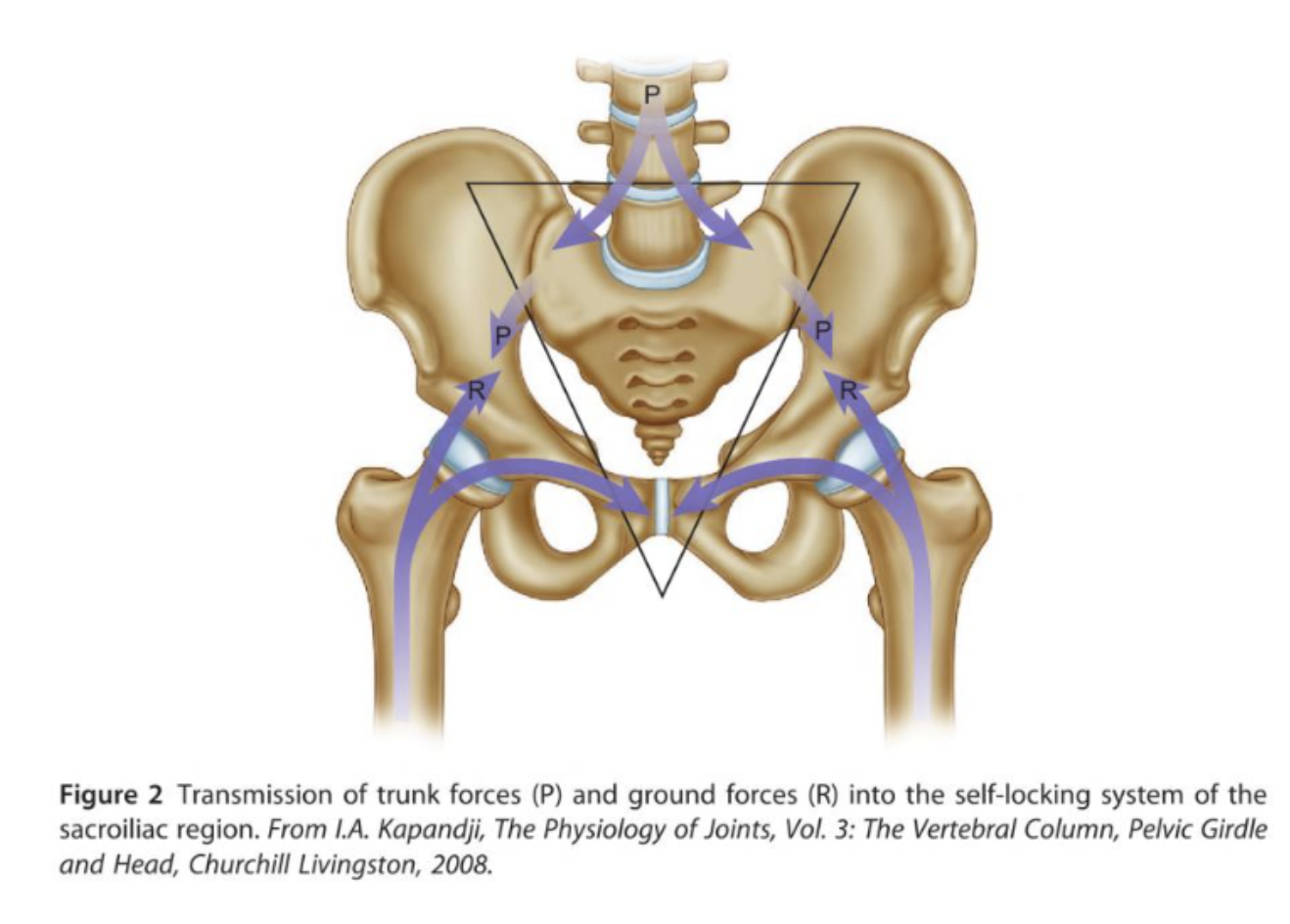
The diagnosis and treatment of the sacroiliac joint (SIJ) can be challenging and is highly debated within the research and among clinicians. While the existing research is focused on investigating variations of mobilizations and manipulations to treat SIJ dysfunction, it is deficient in how to enhance treatment and patient’s self-efficacy with specific exercises. With that in mind, I’ll aim for brevity in my review of the anatomy and biomechanics of the SIJ region so I can focus on existing research and a few “clinical pearls” that I have picked up through my continuing education and practice treating SIJ pain in the clinic. The pelvis can be thought of as a ring or bowl holding our internal organs. The interface between the sacrum (triangular bone at the base of the spine) and ilium bones form the sacroiliac joints. Because of this orientation, the SIJ is well equipped to help manage forces through the pelvis through a combination of bony connections, ligamentous attachments, and muscular attachments. While the sacrum is the attachment point for several major muscle groups (multifidus, erector spinae, latissimus doris, gluteus maximus, piriformis, and portions of the pelvic floor), the sacrum itself does not move in isolation, and it is heavily impacted by muscles attaching in and around the pelvis.
“Non-specific Low Back Pain effects about 60-70% of the population annually.”
How Does the SI joint change over time?
Like many other joints in our body, the SIJ changes throughout our lives, transitioning from relatively mobile in children, to fibrotic and less mobile in adulthood. By our eighth decade of life, studies show about 10% of the population actually have complete ossification and fusion of the SIJ1. Like all joints, the SIJ can develop arthritic changes throughout the lifespan as well, which may or may not contribute to pain. Whether related to trauma, repetitive use, postural dysfunction, or age related changes, the SIJ is a common contributor to low back pain. SIJ is most frequently described as a nagging or sharp pain in the low back or hip, either unilaterally or bilaterally.
What is the recommended treatment of the SI Joint?
The diagnosis and treatment of the SIJ has been controversial because it is a joint with very little motion. Some research suggests it only moves a fraction of a degree, while others suggest it can move up to 7 degrees, depending on the plane of motion2. Relative hyper- or hypo-mobility can both contribute to pain in this area. Regardless of the exact degree to which it can move, the SIJ is capable of such a small amount of movement that it is unlikely to be able to be palpated with high accuracy in a clinical setting whether the joint is rotated or translated. Furthermore, increasing evidence is showing that there is immense variation in the shape of the sacrum from person to person, which would further complicate palpation and being able to detect if the sacrum is not sitting “neutrally” in the joint space3,4. That said, we know that mobilizations and manipulations of the SIJ can be highly successful in treating SIJ dysfunctions based on subjective descriptions of pain locations and objective testing in clinic settings5.
“Chronic lower back pain generators are approximately 40% disc related, 25% facet driven, and 20% Sacroiliac Joint.”
What are the clinic presentations of SI Joint Pain?
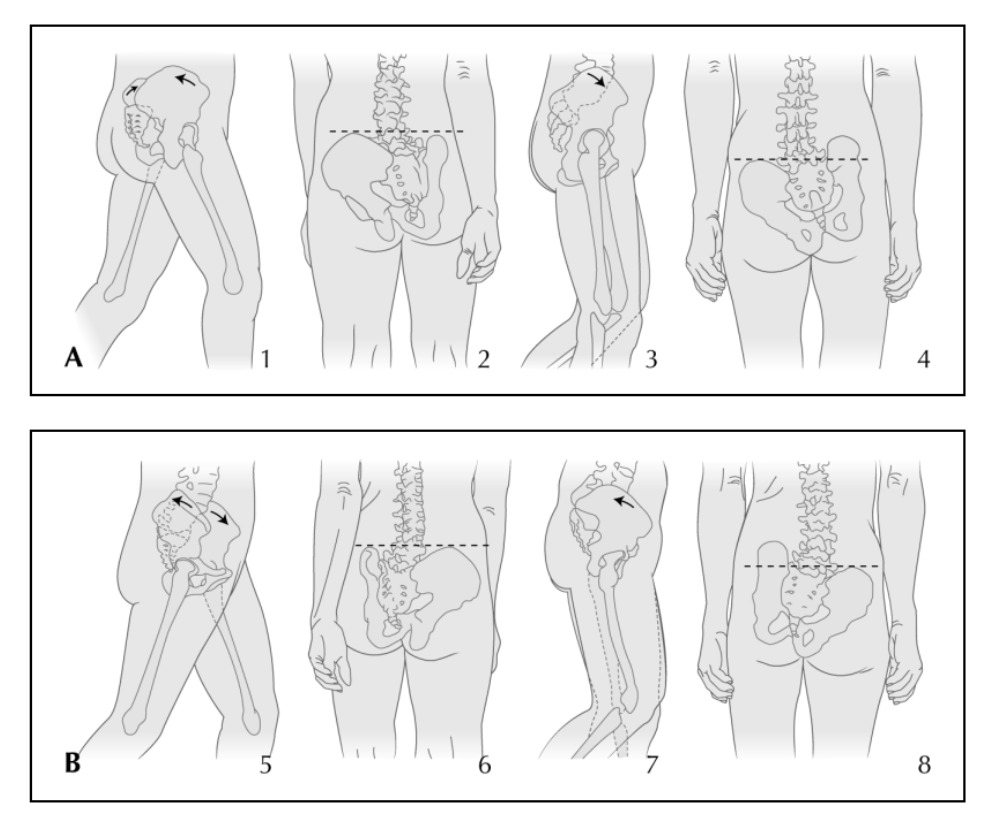
Most commonly in the clinic, I see several common themes arising for my patients with SIJ pain: they often either have difficulty controlling the motion of the pelvis in relation to the low back, or they have difficulty controlling the motion of the pelvis in relation to the femur/leg. Often, we need to address both sides of the equation to see full resolution of symptoms. This may take the form of exercises to address core strength, hip strength, and even foot stability and strength. While we’re addressing biomechanical deficiencies, range of motion, or strength issues above and below the SIJ, we also want to address how the pelvis itself is moving. When dealing with SIJ issues, patients often have limited mobility or stability when moving their pelvis through a certain plane of motion. For example, they may be able to anteriorly and posteriorly tilt their pelvis with minimal difficulty, but rotation is limited on one or both sides. Often, in a clinical setting, I may see patients with this limitation experiencing pain while walking when their leg is extending behind them, preparing for push off. This may be due to poor anterior pelvic tilting on that side, poor posterior pelvic tilt on the opposite side, a lateral hip drop, or difficulty rotating the pelvis. Deficits in any of these motions could lead to the SIJ having to manage forces in a way that it is not accustomed to, and the response may be experiencing pain.
Movement of the pelvis during the gait cycle6
To address these deficits affecting the pelvis and sacrum, I like to follow a few general guidelines:
The better our patients can understand how to move their pelvis, hips, and backs in different functional ways, the better they will feel. Understanding this motion can be very difficult, especially when in pain, because our brains are excellent at compensating and guarding against motions that might reproduce pain. I’ve found it to be very valuable to modify core and hip strengthening exercises so that the patient is lying supine, with their feet pressing into the wall. I’ve noticed that feedback in the form of pressure through the feet quickly changes how a person can translate feeling their body move when laying on their back to feeling it move when standing.
While completing the exercises in the clinic and at home, I recommend starting with a small, pain free range of motion. The SIJ can be highly irritable, and while pushing through pain is rarely successful, neither is skipping an entire exercise. Instead, we can retrain the body through smaller, more comfortable ranges of motion to gradually facilitate normal movement.
Typical SIJ rehab programs focus on core and hip strength, most commonly the transverse abdominis and external rotators of the hip, because we know that these areas are most commonly a weak link along the chain for folks with SIJ pain7. However, I like to emphasize hip internal rotation mobility and strength, especially early on in treatment. By working on improving hip internal rotation, and creating a better balance between the opposing muscle groups, we are able to maximize our ability to generate power with our hip external rotators. We need our muscles to be long and strong all the way through their range of motion, and we can ensure this happens properly by addressing both sides of rotation.
The final area that I often will address with patients with SIJ pain is adductor strength. While it has been shown that individuals with SIJ pain have delayed onset of adductor activation8, adductor strengthening is rarely included in the current literature on SIJ treatment. However, this addition to my SIJ treatment plans has been very helpful, especially for my patients with stubborn or chronic SIJ pain. Similarly to the internal/external rotator relationship, standard SIJ treatments focus heavily on abductor strength, but the adductors play a huge role in pelvis stability and are important to include in an SIJ rehab program.
“In my practice physical therapy, activity modification, rest, and NSAIDs are the foundation of care before we talk about any tier 2 options.”
The SIJ can be a stubborn and recurrent or chronic pain. However, with a close eye, appropriate diagnosis, and specific exercises, the pain can be controlled and often resolved. If you’re struggling with SIJ pain, working with a physical therapist to address biomechanical, strength, or mobility deficits can help.
AUTHOR:
Kerri Smith, PT, DPT, CFSC
LWPT Kirkland Physical Therapist
CONTRIBUTORS:
Dr. Lauren Vernese, DO
Swedish Sport & Spine Physician
Dr. Yung Lee, DO
Evergeen Sport & Spine
Dr. Addison Stone, MD
ProOrtho
Ben Wobker, PT, MSPT, CSCS, CFSC, SFMA
Founder & Director Lake Washington Physical Therapy
Other Blog Articles from Kerri
References:
Neumann, D. A. (2016). Kinesiology of the musculoskeletal system-e-book: foundations for rehabilitation. Elsevier Health Sciences. Pg 361
Goode, A., Hegedus, E. J., Sizer, P., Brismee, J. M., Linberg, A., & Cook, C. E. (2008). Three-dimensional movements of the sacroiliac joint: a systematic review of the literature and assessment of clinical utility. Journal of Manual & Manipulative Therapy, 16(1), 25-38.
Nastoulis, E., Karakasi, M. V., Pavlidis, P., Thomaidis, V., & Fiska, A. (2019). Anatomy and clinical significance of sacral variations: a systematic review. Folia Morphologica, 78(4), 651-667.
Singh, R. (2017). Anatomical variations of sacral hiatus and associated clinical relevance-A review. Int J Anat Var, 4(10), 96-98.
Al-Subahi, M., Alayat, M., Alshehri, M. A., Helal, O., Alhasan, H., Alalawi, A., ... & Alfaqeh, A. (2017). The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: a systematic review. Journal of physical therapy science, 29(9), 1689-1694.
Brolinson, P. G., Kozar, A. J., & Cibor, G. (2003). Sacroiliac joint dysfunction in athletes. Current Sports Medicine Reports, 2(1), 47-56.
Feeney, D. F., Capobianco, R. A., Montgomery, J. R., Morreale, J., Grabowski, A. M., & Enoka, R. M. (2018). Individuals with sacroiliac joint dysfunction display asymmetrical gait and a depressed synergy between muscles providing sacroiliac joint force closure when walking. Journal of Electromyography and Kinesiology, 43, 95-103.
Shadmehr, A., Jafarian, Z., & Talebian, S. (2012). Changes in recruitment of pelvic stabilizer muscles in people with and without sacroiliac joint pain during the active straight-leg-raise test. Journal of back and musculoskeletal rehabilitation, 25(1), 27-32.